What happens when antidepressants are combined with psilocybin?
The short answer is we don’t entirely know but it’s likely safe. The long answer is that we have some preliminary data and some psychopharmacology nuance we can use to make a reasonable guess that generally antidepressants reduce the effects of psilocybin. There have been only 2 randomized clinical trials to date on combining an SSRI and psilocybin and both contained flaws; this means we have much more work to do to better understand how psychiatric and psychedelic treatment approaches play together. Thus far, the research we have done has shown that 1) psilocybin overdose is extremely rare 2) psilocybin does not seem to cause serotonin syndrome 3) higher doses of psilocybin (up to ~60mg) are fairly well tolerated.
How do antidepressant and psilocybin compete with each other?
As you may already know, psilocybin is the psychoactive ingredient in psilocybe mushrooms. Psilocybin is actually not active until is is converted to psilocin which propagates classic psychedelic effects. We often use both psilocin and psilocybin interchangeably, however, when describing psychedelic effects. Psilocin has a multitude of actions, though most relevant to antidepressants is its activation of the 5HT2a (serotonin) receptor in the brain. Antidepressants such as SSRIs, SNRIs, mirtazapine, trazodone, and buspirone, all, to varying degrees, can block psilocin’s target receptor. Also, most importantly, taking antidepressants long-term (weeks to months to years) will result in a compensatory decrease in certain serotonin receptors (5HT2a receptor downregulation), a process of “desensitization” of the serotonin circuitry. This decrease in receptor density may explain why this survey-based study from Hopkins found that long-term ingestion of SSRIs blunt the effects of psilocybin, and whereas this randomized controlled study by Becker et al. that short term ingestion of SSRIs (14 days) did not affect psilocybin’s mystical and psychedelic effects. We see similar blunted effects for other serotonin-dependent psychedelics like LSD ingested among individuals on chronic antidepressants. This blunting phenomenon has recently been systematically academically reviewed by myself and colleagues as well as other scholars. However we need more clinical trials to determine the degree, frequency, and factors that influence this blunting.
What happens in psilocybin clinical trials regarding antidepressants?
Interestingly, the only clinical trial combining long-term SSRIs with psilocybin-assisted therapy was a COMPASS-funded human clinical trial that showed that depressed individuals on SSRIs who received psilocybin-assisted treatment (PAT) had comparable clinical outcomes to those who weren’t on SSRIs and receiving PAT for depression. I say interesting because this is in opposition to other studies on LSD, survey-based data on psilocybin, and frequent clinical anecdote, which has led most clinical trials to require participants to taper off their antidepressant before enrolling in a psilocybin clinical trial.
How much do antidepressants reduce psilocybin’s effects?
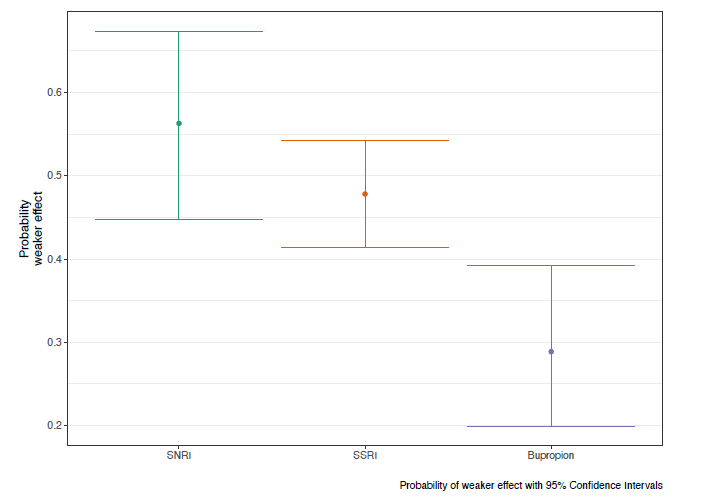
We don’t fully know but much of what we do know if from the survey study mentioned prior by the Hopkins team. Of the 2,625 participants ( 91% white, 55% male, 54% at least had a Bachelor’s degree, and most were located in the USA) who completed the survey and reported taking psilocybin during or after an antidepressant, their reports were filtered down to 596 reports of taking psilocybin with an SSRI, SNRI, or bupropion, that were from 455 survey respondents. They calculated the probability of weaker than expected effects from psilocybin when combined with an antidepressant (most common antidepressants reports were escitalopram (n=146) and sertraline (n=124)) was approximately a coin-toss odds. But could not calculate to what degree the effect would be! Maybe some people feel nothing, maybe other feels something, we simply haven’t studied this yet.
UPDATE: Do less psychedelic effects mean less improvement in mental health outcomes?
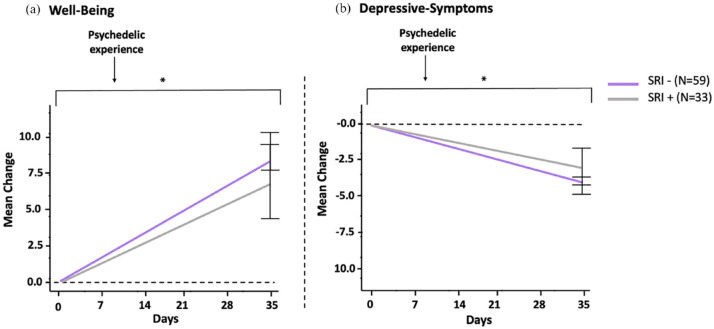
Interestingly, a recent survey study (yes this is data of low rigor, so take with salt!) researchers followed people on an SSRI/SNRI (coded in the image as SRI) from before their ingestion of a psychedelic (mostly psilocybin though other psychedelics were ingested as well among survey respondents), the day after, and then 4 weeks later. They saw that the SSRI/SNRI + psychedelic combination did result in reports of reduced psychedelic effects, but did not appear to reduce the positive effect on depressive symptoms. Notably, although those who were not on an SSRI/SNRI when they ingested a psychedelic had significantly more intense mystical experiences (18.2% more intense), they also had 50.9% more intense challenging experiences and 31.9% more intense emotional breakthroughs.
How is this blunting effect managed?
Again, the Hopkins study found that of those who reported reduced psilocybin effects, 51.7% attempted to overcome this with a higher dose of psilocybin. What we call “compensatory dosing” when someone is on an antidepressant is one strategy. Unfortunately, the highest dose we’ve studied to be safe in a clinical trial setting is ~59mg (~6g of dried psilocybin if going by typical 1% psilocybin content of a psilocybe fruiting body). Psychonauts often will take much higher doses into the irresponsibly named “heroic dosing” range, but as a scientist it’s hard to make much of that on a mass scale. Others may opt to stop their antidepressant the day or so before their dosing session. In this study, there was no significant effect on psilocybin experience from taking an antidepressant holiday. This makes sense since it takes weeks to months to see brain receptors return to baseline after stopping an antidepressant. This very same study found that, and I quote: “this dampening effect on psilocybin effects may last as long as 3 months following antidepressant discontinuation”. This puts many of those seeking treatment in a tough situation; 3 months off antidepressants (a number we can’t even confidently pin down as full wash out off a medication) is a painfully long time to endure potential thoughts of suicide and depression. Plus, it is possible that even without the “trip” there may still be an comparable improvement in depressive symptoms. However, many studies have shown that the trip itself is important in the process of psychedelic-assisted therapy, so there remains much to learn! Be forewarned that many for-profit companies are looking now into a trip-less psychedelic, though it remains to be seen what something like this means for psychedelic forms of healing at large… Regardless, if someone is considering tapering off their antidepressants, I cannot emphasize enough that this is done with appropriate supervision with a trained medical expert. There are numerous risks of coming off an antidepressant. There’s a reason I did 4 more years after medical school to learn about those risks!
What do the researchers think?
While it is common practice to stop taking SRIs at least 2 weeks before the psychedelic experience in recent clinical trials (Carhart-Harris et al., 2016, 2021; Davis et al., 2021; Malcolm & Thomas, 2022), we previously found that discontinuing SRIs before trial start negatively impacted the outcomes, likely due to the emergence of discontinuation symptoms (Erritzoe et al., in press). Additionally, Goodwin et al. (2023) found in an exploratory study that the combination of psilocybin with SSRIs appeared effective and well-tolerated. These findings thus raise the question of whether it might be more prudent to continue subjects on SRIs, possibly at a reduced dose, rather than completely discontinuing them prior to psilocybin-assisted therapy. An alternative approach may entail suggesting patients longer tapering periods with hyperbolic reductions of medication dose (Groot and van Os, 2021; Horowitz and Taylor, 2019) or regimens involving partial tapering focused on dose reduction rather than complete discontinuation. However, this approach also poses challenges, including prolonged treatment gaps prior to psychedelic therapy and might require re-titration of an antidepressant in case of lack of/limited effects of the psychedelic intervention.
So if tapering off has risks and we haven’t studied doses higher than 6g with or without antidepressants on board, then what do I do?
Great question. This is a very nuanced person-by-person answer that requires an extensive skill-set in understanding pharmacology, psychedelic research, antidepressant withdrawal management, psychiatric and medical risk factors identification/management, and contingency planning strategies which will involve, in my opinion, having at least a medical degree and some psychedelic training. These decisions are serious and psilocybin mushrooms are to be respected as extraordinarily powerful tools of healing and harming; your mind and body is to be respected too which means being responsible (lame, I know). I have made it a point to teach other doctors and work with other healers on how to keep people safe. Even so, the ultimate solution is more research and more time.
Thanks for reading and here’s to Nothingness. Mu.

~Dr. S

2 responses to “Psilocybin & Anti-Depressants 💊 Everything You Need to Know (UPDATED 9/2024)”
Thanks for the excellent and thorough discussion!
LikeLike
[…] more information, we recommend this blog post by a leading psychiatrist in Portland, […]
LikeLike